The outbreak of the coronavirus disease has been a rising source of concern among people all over the world. After the coronavirus being well controlled in China, many Chinese medical expertise groups are being sent to those countries including Italy, Iran, Iraq etc where situations are becoming grave. The global increasing number of confirmed cases sparks a huge demand for medical devices. In the fight against COVID-19, ultrasound devices have been playing a critical role.
VINNO Portable Series combines superior image quality, simplified workflow, compact and light weight design all in one. It is a versatile system at the patient bedside offering quick, enhanced mobility and smooth operations even with gloves, greatly enriches the Point of Care.
VINNO Q - Handheld Ultrasound Series is a breakthrough innovation in the ultrasound imaging technology. Its waterproofness, portability, and fast performance make it an outstanding example of how ultrasound devices can help with the Point of Care.
In general, multi frequency, broad-band, harmonic imaging probes of Convex [2-5MHz] and Phased array [1-4MHz] types are preferred. In addition, linear array probe [4-12MHz or 6-16MHz] might be preferred for high resolution imaging in adults and mostly in pediatric imaging. However, for challenging [obese] patients, low frequency probes are preferred to detect pleural effusion or pneumothorax. VINNO offers all the types of probes and frequencies to meet the clinical requirements.

VINNO Portable Machine

(1).jpg)
VINNO Q comes with three probe options
.jpg)
Smooth operation with gloves on
Compact/Point-Of-Care ultrasound products have become one of the most convenient bedside visual imaging methods like a ‘visual stethoscope’, where other imaging modalities have limitations, in the intense fight against this life-threatening disease.

VINNO Compact Series offers a rich set of probes assembled in convex, linear and phased array. The system supports an ultra-broadband frequency of 2-22 MHz to ensure excellent resolution and penetration. In the case of clinical manifestations such as pulmonary infection, acute respiratory distress syndrome (ARDS), pleural effusion, interstitial lung disease, and pulmonary consolidations, VINNO Compact Series can easily and accurately assess the whole-body, especially the cardio-pulmonary function.
I. How to Use Compact Ultrasound for Pulmonary Scanning?
1. What probes can be used for pulmonary ultrasound scanning?
Convex array probe: Offers a scan depth of over 30 cm and a wide field of view.
Linear array probe: Offers a scan depth of up to 4-5 cm and the ability of high resolution lung imaging, sub-pleural consolidations, etc.
Phased array probe: Offers a scan depth of up to 30 cm for cardio-pulmonary function evaluation.
2. What are the commonly used modes for pulmonary ultrasound scanning?
B mode: Displays lung anatomy information, revealing most of the information.
M mode: Dynamically detects how the sampled tissues change over time, mainly intended for observing lung points and diaphragms.
C/PW mode: Observes the blood supply for pulmonary consolidations and assesses cardiovascular blood flow.
3. Implementation protocols
Protocol 1: BLUE-PLUS
(1). Patient positioning
Supine position: Scan the anterior chest wall to detect the pneumothorax. This position is suitable for checking the upper and lower blue points.
Lateral recumbent position: Scan the anterior and lateral chest walls to detect the pleural effusion and pulmonary consolidations. This position is suitable for checking PLAPS (posterolateral alveolar and/or pleural syndrome) point, diaphragm point, and posterior blue point, etc.
Prone position: Keep one side of the patient’s body slightly raised. Scan as much as possible on the dorsal part for small amounts of pleural effusion and small consolidation areas. This position is suitable for checking posterior blue point, PLAPS point, and diaphragm point. See Figure 1 for the gesture for identifying standard points in BLUE-PLUS protocol.
.png)
Gesture for identifying standard points in BLUE-PLUS protocol (1)
Compare the examiner’s hand size with that of the patient, and identify the points based on the patient’s hand size. Except for the two thumbs, the examiner's other eight fingers are close together to cover one side of the chest. The little finger of the upper hand is close to the clavicle, and the fingertips of the two hands are at the anterior midline.
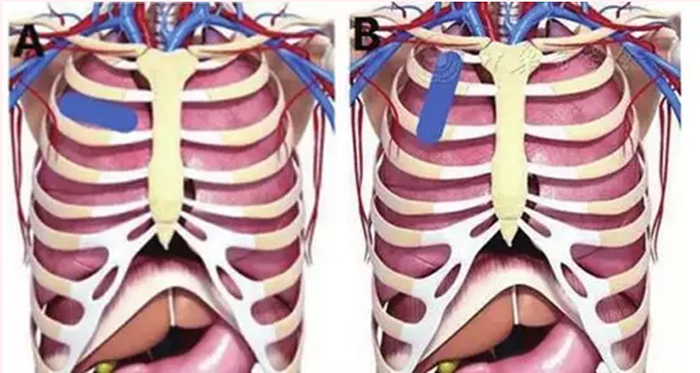
(2). Standard points in BLUE-PLUS protocol (Figure 2)

In Figure 2a, the downward arrow indicates the upper blue point, and the upward arrow indicates the lower blue point. Figures 2b and 2c show how to identify the diaphragm and PLAPS points. Figure 2d indicates the posterior blue point.
Upper blue point: Located between the 3rd and 4th metacarpophalangeal joints of the upper hand.
Lower blue point: Located at the center of the palm of the lower hand.
Diaphragm point: The lower edge of the little finger of the lower hand constitutes the diaphragm line, and the diaphragm point is located where the rearward extension of the diaphragm line intersects with the midaxillary line.
PLAPS point: Located at where the rearward extension of the lower blue point intersects with the posterior axillary line.
Posterior blue point: Located in the area between the scapular line and the spine.
(3). Scanning method
Place the probe in the intercostal space of the five standard points identified in the BLUE-PLUS protocol. Then perform a transverse scan (with probe parallel to the intercostal space, as shown in Figure 3a) and a longitudinal scan (with the probe perpendicular to the intercostal space, as shown in Figure 3b) at each point. It is advisable that the probe be directed toward the sternum of the anterior chest when scanning at the PLAPS point. You can also scan the body surface projection area that covers the lesion area indicated by the CT exam, and then make a mark and save the image.
Transverse scan ( left); Longitudinal scan ( right).
Mark the images at each point to facilitate remote consultation. Mark the images as follows: Mark the upper blue point as 1, the lower blue point as 2, the diaphragm point as 3, the PLAPS point as 4, and the posterior blue point as 5, and then mark the left and right parts. For instance, the image at the right upper blue point should be marked as R1.
Protocol 2: One Lung with Six Regions
The lung is divided into six regions: two anterior, two lateral, and two posteriors, according to anatomical landmarks set by anterior and posterior axillary lines. Each region is divided in half: superior and inferior. Quickly perform transverse and longitudinal scans based on the clinical manifestations and predilection sites of the patient.

(1) Anterior chest scan: The patient takes a supine or semi-recumbent position. The scan is mainly intended for checking for pneumothorax.
(2) Lateral chest scan: The patient takes a supine or semi-recumbent position. The scan is mainly intended for checking for atelectasis or consolidations.
(3) Posterior chest scan: The patient takes a supine or a slightly lateral recumbent position. The scan is mainly intended for checking for pulmonary pleural effusion or pulmonary edema.
II. Common Signs of Pulmonary Ultrasound Scanning
1. Pleural line and A-line
Pleural line: The pleural line is a smooth, regular, hyperechoic line located 0.5 cm below the rib line.
A-line: In a normal aerated lung, hyperechoic, horizontal lines arising at regular intervals from the pleural line can be seen, which are called A-lines.

Ultrasound signs of pleural line and A-line
2.The bat sign: In 2D ultrasound imaging, the pleural line and the adjacent ribs outline a silhouette reminiscent of a bat, which is called the bat sign.

The bat sign
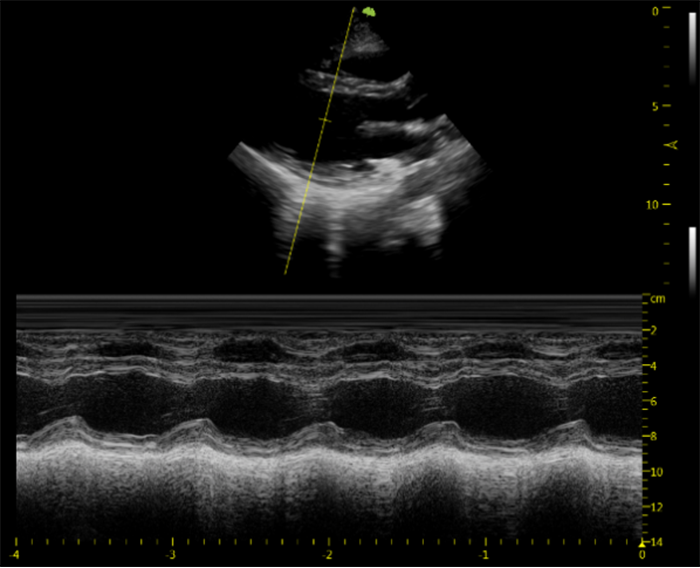
3.The pleural sliding sign: The relative motion of the visceral pleura with the parietal pleura in association with respiration.
4.The seashore/sandy beach sign: This phenomenon would be observed in the M-mode ultrasound image of a normal lung. The lung echoes of the pleural line is granular due to the presence of pleural sliding, which looks like the beach on the coast; the parallel lines formed by the soft tissues in the anterior chest wall represent the sea.

The seashore/sandy beach sign
5.B-line: B-lines are defined as comet-tail artifacts that arise from the pleural line, travel perpendicular to the pleural line, and extend to the entire imaging depth. A small number, no more than three, of B-lines may be detected in a normal lung. B-lines have seven unique features: comet-tail artifacts, arising from the pleural line, hyperechoic, laser-like, without fading, and extending to the bottom of the screen.

B-Line
6.Pleural effusion

III. What Else Ultrasound Can Help Critically Ill Patients?
1. Acute respiratory distress syndrome (ARDS): ARDS is a common type of respiratory failure, and mechanical ventilation is always required for patients with ARDS. In addition to diagnosis, ultrasound can also guide how to set up PEEP and how to improve pulmonary ventilation function based on the changes in the number of B-lines, changes in spacing, and dynamic bronchial signs.
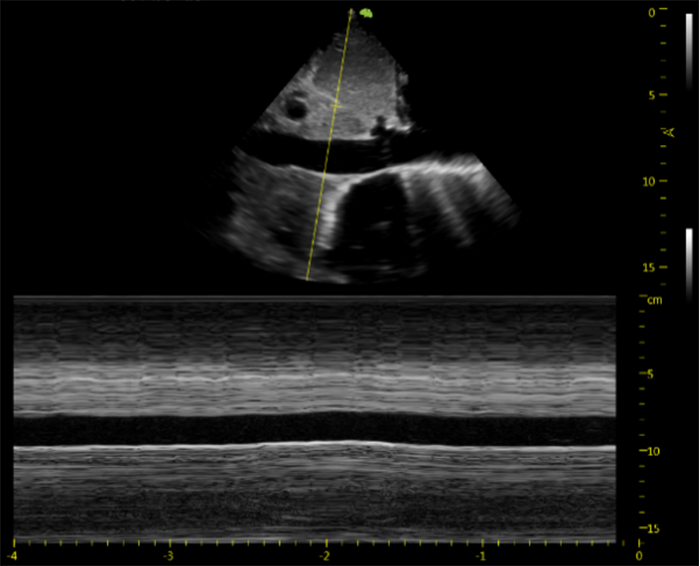
2. Volume responsiveness assessment: The main purpose of blood volume assessment is to determine whether the patient needs rapid fluid replacement and whether the fluid replacement is effective. The assessment can be performed against these two criteria: 1) stroke volume or cardiac output; 2) the internal diameter of the inferior vena cava and its changes with respiration, both can be easily assessed and followed at point of care using VINNO compact ultrasound series.


IV. Image Storage
1. Collect dynamic images for each standard point, at least one each for transverse and longitudinal scans.
2. Make sure the storage time of dynamic images is longer than 3-5 seconds.
3. Store static images within the measured lesions (consolidations and pleural effusion).
The ongoing battle against the Coronavirus outbreak has raised the bar higher on the comprehensive treatment capabilities on the front line as well as profession-specific diagnostic aids. With a light and compact structure and the ability to deliver high-quality imaging, VINNO Portable and Q series can respond quickly to emergent and high-risk situations, thereby empowering physicians with ways of seizing the best timing for treatment.
REFERENCE
Reprinted from “Lung Ultrasound Protocol for Diagnosis of 2019-nCoV Pneumonia and Remote Consultation”.

